Is It Easy to Drive Along 101
Narcolepsy 101: Signs, Causes and Treatments
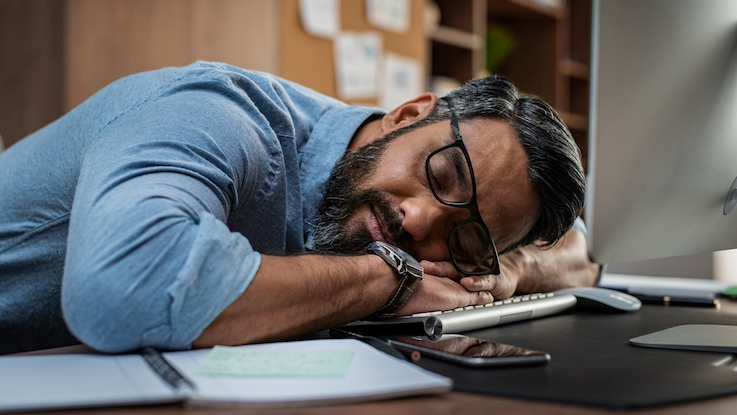
Narcolepsy is a chronic (long-term) sleep disorder. It disrupts the brain's control over normal sleep-wake cycles. This makes you feel drowsy during the day and can make you fall asleep at inappropriate times — like when you're at work.
Normally, when you fall asleep, you go through a phase called non-rapid eye movement (NREM) sleep where your brain waves start to slow down. Then after an hour or so, you enter the deeper phase of rapid eye movement (REM) sleep.
If you have narcolepsy, you may skip over NREM and enter suddenly into REM sleep. This means the changes that usually happen during deep sleep (like extreme sleepiness, muscle weakness and dreaming) start happening when you're awake during the day.
Narcolepsy is a fairly rare condition. It affects around 200,000 people in the United States, and roughly 1 in every 2,000 people worldwide. But many people with narcolepsy don't know they have it — so the real numbers may be higher.
Having narcolepsy can disrupt your daily life. But the good news is there are treatments that can help. Learn more about the symptoms and causes of narcolepsy and how to get treatment.
The main symptoms of narcolepsy are problems with sleeping at night and falling asleep suddenly during the day. Common signs of narcolepsy include:
- Feeling very drowsy during the day and having trouble staying awake and alert
- Falling asleep suddenly at inappropriate times
- Falling asleep for just a few seconds while doing an activity like eating, talking or driving — but continuing to do the activity
- Trouble sleeping solidly through the night
- Being unable to move or speak when waking up or falling asleep (called sleep paralysis)
- Vivid dreaming or hallucinations when you're falling asleep or waking up
- Trouble remembering things that happened during the day (because you weren't fully awake at the time)
Some people with narcolepsy also have cataplexy (sudden loss of muscle tone). Cataplexy makes you feel very weak all of a sudden, so that you can't stand or hold your head up. It's often triggered by a strong emotion like laughter, stress or anger.
There are 2 types of narcolepsy:
- Type 1 narcolepsy (previously called narcolepsy with cataplexy) — People with type 1 either have cataplexy symptoms, or they have low levels of a brain hormone called hypocretin that controls sleep-wake cycles.
- Type 2 narcolepsy (previously called narcolepsy without cataplexy) — People with type 2 don't have cataplexy and have normal levels of hypocretin. Their symptoms are usually less severe overall.
Causes of Narcolepsy
The exact cause of narcolepsy is unknown. Current research suggests that narcolepsy most likely happens through a combination of genetic and environmental factors. Possible causes include:
- Autoimmune problems — Most research points to narcolepsy being an autoimmune problem, meaning that the immune system mistakenly attacks healthy cells or tissues. In people with type 1 narcolepsy, the immune system may destroy the brain cells that produce hypocretin or the receptors that allow it to work.
- Family history — Around 1 in 10 people with narcolepsy have a close relative with similar symptoms. Studies suggest your risk of narcolepsy is 20 to 40 times higher if you have a family member with narcolepsy.
- Brain injuries — In rare cases, narcolepsy can happen after a traumatic brain injury or tumor in the region of the brain that regulates sleep-wake cycles.
Diagnosing Narcolepsy
Narcolepsy can develop at any age. Symptoms most often begin during the teen years, but it often takes several years or even decades to get a diagnosis. Symptoms may appear one at a time, several years apart, which makes it harder to diagnose.
Your primary care doctor can make a preliminary diagnosis based on your symptoms. But you'll need to see a sleep specialist to get a final diagnosis. The specialist will ask about your medical history and family health history. You may also need to stay overnight at a sleep center for special tests.
Tests and methods for diagnosing narcolepsy include:
- Sleep history — Your doctor may ask you to answer a questionnaire called the Epworth Sleepiness Scale. You use a numbered scale to rate how likely it is that you would doze off in different situations.
- Sleep record — You may need to keep a diary or sleep log to record your regular sleep pattern for a week or two. Your doctor may also ask you to wear an actigraph — a wristwatch-like tool that measures when and how much you move during sleep.
- Polysomnogram (PSG) — For this test, you'll stay overnight at a sleep facility. Your doctor will use electrodes to measure the electrical activity of your brain and heart during sleep. They'll also measure how much your muscles and eyes move while you're asleep.
- Multiple sleep latency test (MSLT) — This is a daytime sleep test. You'll take several naps 2 hours apart while a specialist observes your sleep pattern and measures how long it takes you to fall asleep.
- Hypocretin level — To test the level of this brain hormone, your doctor will take a sample of spinal fluid from your lower back.
Treatments for Narcolepsy
There's currently no cure for narcolepsy. But medicines and lifestyle changes can help you manage your symptoms and improve your daily life.
Medicines
Your doctor may prescribe medicines that help reduce daytime sleepiness, including:
- Modafinil — This is a stimulant medicine that can reduce daytime sleepiness and make you feel more alert. It's one of the most commonly used narcolepsy medicines because it's less addictive and has fewer side effects than other narcolepsy drugs.
- Other stimulants — If modafinil doesn't work, doctors may prescribe amphetamine-like stimulants. These have several known side effects including irritability, heart rhythm changes, shaking and trouble sleeping at night.
If you have type 1 narcolepsy with cataplexy, your doctor may recommend other medicines to help with that symptom, including:
- Antidepressants — Certain types of antidepressants can help with cataplexy. Antidepressants can cause side effects, including high blood pressure and changes in heart rhythm.
- Sodium oxybate — This is a strong sedative that you take twice a night. Doctors only prescribe this medicine in severe cases where other medicines haven't worked.
Talk with your doctor about the risks and benefits of each treatment option. Together you can find a treatment plan that's right for you.
Lifestyle changes
Medicines alone may not be enough to control the symptoms of narcolepsy. For best results, you can combine medicines with lifestyle changes that promote better sleep. Try these tips:
- Take short naps throughout the day. Brief naps throughout the day can help manage daytime sleepiness. Of course, school and work commitments can make napping difficult. Your doctor can provide a recommended sleep schedule to help you work out a plan with your school or employer.
- Get regular physical activity. Aim for at least 20 minutes of activity a day. Try to finish exercising at least 4 to 5 hours before bedtime.
- Stick to a regular sleep schedule. To help regulate your body's sleep cycle, get into a routine of going to bed and waking up at the same time each day.
- Relax and wind down before bed. Make sure your bedroom is quiet and at a comfortable sleeping temperature. Try to do something relaxing about an hour before bedtime, like taking a bath, reading a book or listening to a soothing podcast.
- Avoid caffeine, alcohol and heavy meals before bed. Try not to have caffeinated drinks after midday. And avoid drinking alcohol or having heavy meals for several hours before bedtime.
Your Next Steps
If you think you have symptoms of narcolepsy, you can do a quick self-test by asking yourself the following questions:
- Do you ever have the sudden urge to sleep during the day — even though you're getting enough sleep at night?
- After a nap, do you feel alert for a short time but then start to feel very sleepy again?
- Do you feel so sleepy during the day that it disrupts your personal or work life (like dozing off while working, eating or talking to someone)?
If the answer to any of these questions is yes, talk with your doctor. It's also helpful to keep notes about your symptoms and sleep patterns before your doctor's visit. That way, your doctor can get a better idea of your situation and refer you to a sleep specialist if needed.
Resource Links:
- "Narcolepsy" via National Health Service
- "Narcolepsy" via Mayo Clinic
- "Narcolepsy" via MedlinePlus Genetics
- "Narcolepsy" via NORD (National Organization for Rare Disorders)
- "Narcolepsy" via Sleep Education by American Academy of Sleep Medicine
- "Narcolepsy Fact Sheet" via National Institute of Neurological Disorders and Stroke
Source: https://www.symptomfind.com/health-conditions/narcolepsy-condition?utm_content=params%3Ao%3D740013%26ad%3DdirN%26qo%3DserpIndex&ueid=4b946939-67a5-4ebb-a9ed-8a800e16f6d4
0 Response to "Is It Easy to Drive Along 101"
Post a Comment